Provision of Audiologic Care in Nursing Homes: A Study of In-service Training with Facility Staff Members
Lamb HB 1,2, Jones AL1
1Department of Communication Disorders, Auburn University, United States
2Atlanta Hearing Associates, Georgia, United States
- *Corresponding author: Alisha L. Jones, Department of Communication Disorders, Auburn University, 1199 Haley Center, Auburn, Alabama 36839.
-
Article Details
Received: Dec 07, 2016; Accepted: Jan 24, 2017; Published: Jan 26, 2017
-
Competing Interests
The authors have declared that no competing interests exist.
-
Cite as:
Lamb HB, Jones AL. Provision of Audiologic Care in Nursing Homes: A Study of In-service Training with Facility Staff Members. J Commun Disorder Assist Technol. 2017; 1: 1-17.
-
Creative Commons Attribution License
This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
-
Key Words
Education and Training, Hearing Loss, Nursing Homes
ABSTRACT
Objectives: To investigate knowledge of nursing home staff members regarding hearing loss topics in the elderly.
Method: An educational training presentation was designed to determine if a single in-service training yielded significant improvement in audiological competency among nursing home staff members as related to self-perceived confidence working with residents with hearing impairment. An online survey was administered prior to and following the training.
Results: Post-training survey responses indicated significant improvement in personal confidence regarding hearing loss and training with hearing aids.
Discussion: Education regarding hearing loss topics in the elderly should be a part of training for nursing home and assisted living facility staff to improve communication between the residents with hearing impairment and staff.
INTRODUCTION
As the U.S. population rapidly ages, provision of efficient and effective healthcare for the elderly is becoming increasingly necessary in the field of audiology. The U.S. Bureau of the Census reported that 13% of the current total population was over 65 years of age, and by the year 2050 this age group will comprise over 20.9% of the total population [1]. A report by the American Association of Retired Persons in 2007 indicated that the population over age 65 living in nursing homes will double by 2020 [2]. The American Speech-Language-Hearing Association reported in 1988 that an estimated 70-80% of nursing home residents have a measurable hearing impairment. These findings support the necessity for nursing home staff members to possess a good general understanding of how to communicate with and provide care for residents with hearing impairment [3].
With an estimated 46% of nursing home residents having been diagnosed with some form of dementia, identification of hearing loss in this population is critical, as undetected and untreated hearing loss can mimic cognitive impairments [2,4,5]. The combination of hearing impairment and cognitive decline due to aging jeopardizes an individual’s ability to comprehend and adhere to healthcare provider recommendations and instructions, thereby compromising the integrity of healthcare services provided to the geriatric population, including physical exams, cognitive training, speech therapy, and physical rehabilitation [2,4].
Changes in quality of life including depression, reduced independence, and poor health have been associated with hearing loss in older adults [6]. Nursing home residents who have not received appropriate audiological services may experience social isolation, cognitive decline, and decreased mobility resulting in increased behavioral agitation [2]. Studies have shown that improved communication between staff and residents had a positive impact on residents’ quality of life, and that amplified hearing resulted in improvements in mood, social interactions, and performances on daily living tasks [7].
With the majority of the elderly population acquiring hearing loss due to aging, it is increasingly important for caregivers to understand the characteristics of this type of hearing loss, also known as Presbycusis. Adults with Presbycusis have normal to near-normal hearing in the low frequency range, with hearing sensitivity decreasing in the mid-to-high frequencies. Background noise is typically centered in the low-frequency range, while speech signals responsible for consonants that provide clarity and understanding of speech are centered in the mid-tohigh frequency range. Presbycusis has an adverse reaction on communication, affecting an individual’s ability to understand speech in noisy or reverberant environments, as they are able to hear the background noise but not the speech signal. In later stages of presbycusis, the individual’s ability to localize sounds is also impacted [8].
ALDs are used to improve communication with individuals with a hearing loss severity ranging from mild to profound, as well as individuals with normal hearing acuity who have learning disabilities, central auditory processing disorders, or cognitive impairments. ALDs are highly versatile as they can be used in large or small groups, alone or in conjunction with personal hearing aids, and easily transported or permanently installed. Because ALDs maintain a clear presentation of the speech signal in the presence of poor room acoustics, residents will achieve better communication with staff members and increased/improved personal safety despite the handicap caused by hearing loss in the presence of excessive noise, reverberation, and distance between the listener and sound source [9].
In order to identify individuals who would likely benefit from ALDs, hearing handicap scales and questionnaires may be administered to aid in the identification of hearing problems among nursing home residents. Although these questionnaires serve as useful screening tools, they are often not completed by audiologists in nursing homes due to time constraints. It is ideal for nursing staff members to complete a staff member hearing handicap scale, due to their familiarity with the resident’s communication style and unique ability to observe the resident in a variety of informal listening situations. Handicap scales provide information regarding how others perceive the effects of hearing impairment on the resident’s quality of life while helping to identify the need for audiologic intervention [4]. If hearing impairment is identified, a resident may be a candidate for hearing aids or an assistive listening device such as a Pocket talker, which can assist nursing staff members and therapists during conversations and therapy sessions [9].
Due to the high turnover rate among nursing home staff members, ongoing staff training regarding hearing healthcare is critical. A study conducted by Cohen-Mansfield and Taylor [10] examined barriers to hearing aid use among persons reported to have hearing aids and among those reported to have hearing difficulties but no hearing aids in a nursing home facility. Interviews were conducted with both nursing home residents and nursing staff members to obtain information regarding the residents’ hearing ability, hearing aid use and daily maintenance, and potential barriers to use. Results indicated that sixty-nine percent of residents who used a hearing aid reported problems with the device and eight-six percent of residents reported needing help taking care of the hearing aids. Approximately half of the staff members interviewed reported having not received any training in the use or maintenance of the hearing aid devices, and it was reported that relatives were used for maintenance of hearing aids in fourteen percent of residents with hearing aids. While studies such as Cohen-Mansfield and Taylor [10] suggest that the barriers to hearing aid use among residents in nursing home facilities are multifactorial, results support commitment to staff member education. This education should include components regarding hearing loss identification, care procedures, hearing aid design, and fit issues which play a crucial role in the successful utilization of hearing aids and in turn communication among nursing home residents.
The current study was proposed to investigate attitudes and knowledge of nursing home staff members regarding hearing loss, hearing aids, ALDs, and environmental accommodations for hearing impaired residents. An educational training presentation was designed for a single in-service training and the study evaluated if significant improvement in audiological awareness among nursing home staff members as related to self-perceived confidence working with hearing impaired residents following the in-service training. These audiological competencies included making environmental accommodations, troubleshooting and maintenance of amplification devices, and familiarity with appropriate audiological referral protocol.
DESIGN AND METHOD
Participants were nursing staff members presently employed at Covenant Woods of Gardendale assisted living facility, in Gardendale, Alabama. A group of 35 adults participated in the first survey. A group of 26 adults participated in the second survey. There was a loss of participants between the first and second survey. All participants were female adults over 18 years of age. Participants reported various formal educational backgrounds and various years of experience caring for individuals with hearing impairment. The Institutional Review Board (IRB) of Auburn University approved this study.
An audiology in-service presentation was developed for this study that included information on basic anatomy and physiology of the ear, types of hearing loss, communication strategies, assistive listening devices, use of questionnaires, referrals, and hearing aid styles, components, and maintenance. A 25-item closed question survey entitled, “Nursing Home Staff Survey: Part I” was developed. Topics of the survey included demographics, education levels, current knowledge about hearing loss, referral protocol for hearing loss and hearing instrument-related concerns, hearing technology and devices, and special accommodations for common listening environments in nursing homes. A 20-item closed question survey entitled, “Nursing Home Staff Survey: Part II” was developed to be given following the training. Topics of the second survey included topics and questions addressed in the first survey to observe the perceived benefit received from the in-service training, as well as future considerations for management of residents with hearing loss. Qualtrics survey website was used to submit and collect online survey response items anonymously.
Procedure
Using a list-serve of email addresses for all nursing staff employees of Covenant Woods of Gardendale assisted living facility, an informational letter was sent electronically by the executive director explaining the purpose and procedure of the present study. As explained by the nursing staff director, nursing staff employee attendance was mandatory for all in-service trainings scheduled by Covenant Woods of Gardendale scheduled during regular work hours. A link to the online survey to take prior to the mandatory in-service training was included in the informational letter if the employee chose to participate in the study anonymously.
The in-service training on hearing loss and listening technology designed for the study was scheduled for March 17, 2015 as one of several in-service training topics assigned by Covenant Woods of Gardendale for the calendar year. The first informational letter and survey link was emailed to nursing staff on March 2, 2015, and was made accessible through March 16, 2015. The second informational letter and survey link was emailed to nursing staff on March 18, 2015, and was made accessible through March 31, 2015. The content for the second informational letter was the same as the content for first informational letter. Each survey estimated an approximate 15-minute completion time. Survey response items were collected through anonymous submission of surveys through the Qualtrics website. Data was analyzed based on the subjects’ survey response prior to and following the in-service training for comparison and trend identification among all participants. Repeated measures analysis of variance (ANOVA) were used to analyze pre and post surveys.
RESULTS AND DISCUSSION
Initial Survey Results
Results from the initial survey gave the background of the respondents and attitudes towards hearing health care. Fifty percent of respondents reported having received formal education regarding the care of individuals with hearing impairment and 50% reported not having received formal education regarding the care of individuals with hearing impairment. Forty-two percent of respondents reported 1-2 years experience caring for persons with hearing impairment. Nineteen percent of respondents reported 3-5 years of experience caring for persons with hearing impairment. Nineteen percent of respondents reported 6-10 years of experience caring for persons with hearing impairment. Nineteen percent of respondents reported greater than 10 years of experience caring for persons with hearing impairment.
Twenty percent of respondents reported they strongly agree that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial. Fifty-four percent of respondents reported they agree that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial. Eleven percent of respondents reported they neither agree nor disagree that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial. Nine percent of respondents reported they disagree that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial. Six percent of respondents reported they strongly disagree that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial.
Thirty-seven percent of respondents reported that a seminar would definitely influence their care of nursing home residents with hearing impairment. Forty-three percent of respondents reported that a seminar would probably influence their care of nursing home residents with hearing impairment. Twenty percent of respondents reported that a seminar would maybe influence their care of nursing home residents with hearing impairment. Overall, the majority of respondents reported that a seminar would be likely to influence their care of nursing home residents with hearing impairment.
Thirty-four percent of respondents reported they would be very likely and thirty-one percent of respondents reported they would be likely to attend to a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment. Seventeen percent of respondents reported they would be undecided to attend to a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment. Three percent of respondents reported they would be unlikely to attend to a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment Fourteen percent of respondents reported they would be very unlikely to attend to a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment. Overall, the majority of respondents reported they would be more likely than not to attend to a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment.
Comparison of Pre-Survey and Post-Survey Data
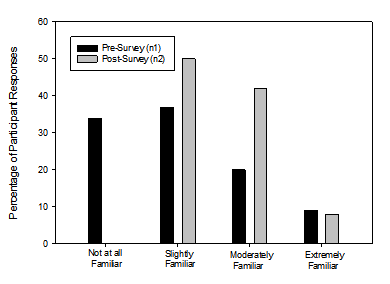
The majority of pre-survey participants reported they were “slightly familiar” while the majority of post-survey participants reported “moderately familiar” regarding the different styles of hearing aids. A one way repeated measures analysis of variance (ANOVA) was completed for the question “How familiar are you with the different styles of hearing aids?” This was statistically significant (F [3, 61] = 2.75, p < 0.05) and showed an overall increase in familiarity with the different styles of hearing aids. The distribution of responses from all participants is shown in Figure 1. [/mp_text] [/mp_span] [/mp_row] [mp_row] [mp_span col="12"] [mp_image id="3506" size="full" link_type="media_file" link="#" target="false" caption="false" align="center"] [/mp_span] [/mp_row] [mp_row] [mp_span col="12"] [mp_row_inner] [mp_span_inner col="12"] [mp_text] [/mp_text] [/mp_span_inner] [/mp_row_inner] [mp_row_inner] [mp_span_inner col="12"] [mp_text]
Figure 1: Responses to the question: How familiar are you with the different styles of hearing aids (behind-the-ear, in-the-ear, receiver-in-the-ear, etc.)?
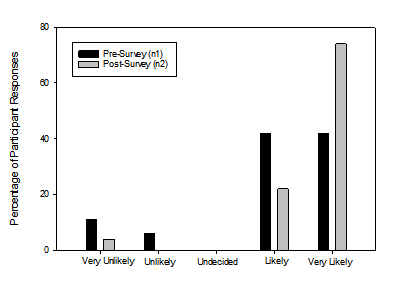
[/mp_span_inner] [/mp_row_inner]The majority of pre-survey participants reported feeling “slightly confident” while the majority of post-survey participants reported feeling “moderately confident” regarding how to make appropriate hearing loss and/or amplification referrals. A one way repeated measures ANOVA was completed for the question “How confident do you feel regarding how to make appropriate hearing loss/amplification referrals?” This was statistically significant (F [3, 61] = 2.83, p < 0.05) and showed an overall increase in confidence for making referrals. The distribution of responses from all participants is shown in Figure 2. [/mp_text] [/mp_span_inner] [/mp_row_inner] [/mp_span] [/mp_row] [mp_row] [mp_span col="12"] [mp_row_inner] [mp_span_inner col="12"] [mp_text] The majority of both pre-survey and post-survey participants reported feeling “slightly confident” regarding when to make appropriate hearing loss and/or amplification referrals. A one way repeated measures ANOVA was completed for the question “How confident do you feel regarding when to make appropriate hearing loss/amplification referrals?” This was statistically significant (F [3, 61] = 4.66, p < 0.01) with an increase in participants rating that they were moderately confident post training. The distribution of responses from all participants is shown in Figure 3. [/mp_text] [/mp_span_inner] [/mp_row_inner] [mp_row_inner] [mp_span_inner col="12"] [mp_image id="3507" size="full" link_type="custom_url" link="#" target="false" caption="false" align="center"] [/mp_span_inner] [/mp_row_inner] [mp_row_inner] [mp_span_inner col="12"] [mp_text] Figure 2: Responses to the question: How confident do you feel regarding how to make appropriate hearing loss and/or amplification referrals?
Figure 3: Responses to the question: How confident do you feel regarding when to make appropriate hearing loss and/or amplification referrals?
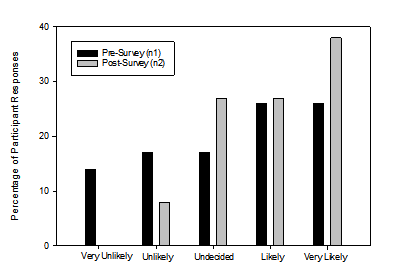
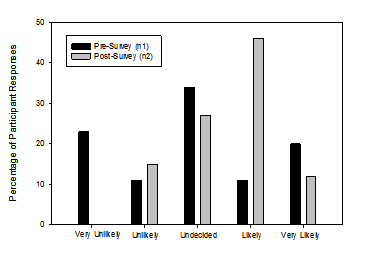
An equal number of pre-survey participants reported they would be “likely” or “very likely” while the bulk of post-survey participants reported they would be “very likely” to check if a resident is wearing their hearing aids. A one way repeated measures ANOVA was completed for the question “How likely are you to check if a resident is wearing their hearing aids?” This was not statistically significant (F [3, 61] = 2.18, p = 0.10). The distribution of responses from all participants is shown in Figure 4.
Figure 4: Responses to the question: How likely are you to check if a resident is wearing their hearing aids?
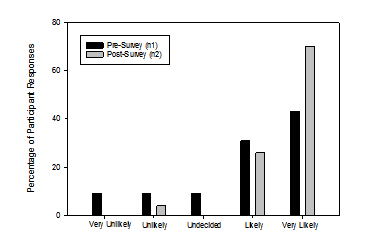
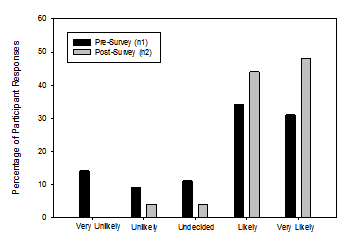
The greater part of pre-survey participants reported they would be “likely” while the greater part of post-survey participants reported they would be “very likely” to check if a resident’s hearing aid or assistive listening device is turned on. A one way repeated measures ANOVA was completed for the question “How likely are you to check if a resident’s hearing aid or assistive listening device is turned on?” This was not statistically significant (F [4, 60] = 2.18, p = 0.08). The distribution of responses from all participants is shown in Figure 5.
Figure 5: Responses to the question: How likely are you to check if a resident’s hearing aid or assistive listening device is turned on?
Figure 6: Responses to the question: How likely are you to clean and/or remove ear wax from a resident’s hearing aid?
The majority of both pre-survey and post-survey participants reported they would be “very likely” to change the battery in a resident’s hearing aid. A one way repeated measures ANOVA was completed for the question “How likely are you to change the battery in a resident’s hearing aid?” This was not statistically significant (F [4, 61] = 2.05, p = 0.10). The distribution of responses from all participants is shown in Figure 7.
Figure 7: Responses to the question: How likely are you to change the battery in a resident’s hearing aid?
The greater part of pre-survey participants reported they were “undecided” while the majority of post-survey participants reported they would be “likely” to change a dome or wax filter on a resident’s hearing aid. A one way repeated measures ANOVA was completed for the question “How likely are you to change a dome or wax filter on a resident’s hearing aid?” This was statistically significant (F [4, 61] = 4.13, p < 0.01). The distribution of responses from all participants is shown in Figure 8.
Figure 8: Responses to the question: How likely are you to change a dome or wax filter on a resident’s hearing aid?
The majority of pre-survey participants reported they would be “likely,” while the majority of post-survey participants reported they would be “very likely” to conduct a listening check of a resident’s hearing aid or assistive listening device. A one way repeated measures ANOVA was completed for the question “How likely are you to conduct a listening check of a resident’s hearing aid or assistive listening device?” This was not statistically significant (F [4, 61] = 2.14, p = 0.09). The distribution of responses from all participants is shown in Figure 9.
Figure 9: Responses to the question: How likely are you to conduct a listening check of a resident’s hearing aid or assistive listening device?
Participants rated their familiarity with different types of amplification and assistive listening devices. For part A of the question, in which familiarity with hearing aids was rated, a one way repeated measures ANOVA was completed, and showed no statistical significance between pre and post training (F [4, 61] = 1.89, p = 0.12). A one way repeated measures ANOVA was completed for part B of the question, in which familiarity with cochlear implants was rated, and showed statistical significance between pre and post training (F [3, 61] = 4.42, p < 0.01). A one way repeated measures ANOVA was completed for part C of the question, in which familiarity with personal FM systems was rated, and was statistically significant between pre and post training (F [3, 61] = 6.95, p < 0.00). A one way repeated measures ANOVA was completed for part D of the question, in which familiarity with an amplified telephone was rated, and was statistically significant between pre and post training(F [3, 61] = 3.20, p < 0.03). A one way repeated measures ANOVA was completed for part E of the question, in which familiarity with a TV streamer was rated, and was statistically significant between pre and post training (F [3, 61] = 6.70, p < 0.00). A one way repeated measures ANOVA was completed for part F of the question, in which familiarity with a soundfield FM system was rated, and was statistically significant between pre and post training (F [3, 61] = 11.61, p < 0.00). Overall, the majority of participants reported increased familiarity with hearing aids, cochlear implants, personal FM systems, amplified telephones, TV streamers, and Soundfield FM systems following the in-service training. Increased familiarity observed across pre and post survey responses was statistically significant for all test items except hearing aids at the p > .05 level.
Participants rated their preparedness to carry out appropriate protocols in four different situations. A one way repeated measures ANOVA was completed for part A of the question, in which protocol for a missing device was rated and was not statistically significant (F [3, 61] = 1.54, p = 0.22). A one way repeated measures ANOVA was completed for part B of the question, in which protocol for a broken device was rated and was not statistically significant (F [3, 61] = 2.34, p = 0.08). A one way repeated measures ANOVA was completed for part C of the question, in which protocol if hearing loss is suspected by a resident or family member was rated and was not statistically significant (F [3, 61] = 0.88, p = 0.46). A one way repeated measures ANOVA was completed for part D of the question, in which protocol if the staff suspects the resident has hearing loss was rated and was not statistically significant (F [3, 61] = 1.34, p = 0.27). Overall, increased self-perceived preparedness observed across pre- and post- survey responses were not statistically significant for all test items at the p > .05 level.
Second Survey Results
Responses from the second survey revealed attitudes regarding the in-service training. For the question “Do you agree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents?”, thirty-five percent of participants reported they strongly agree and forty-six percent participants reported they agree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents. Fifteen percent of participants reported they neither agree nor disagree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents. Four percent of participants reported they strongly disagree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents. Overall, the majority of participants reported they agree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents. The distribution of responses from all participants is shown in Table 1.
For the question “How likely are you implement environmental modifications with hearing impaired residents in the future?”, twenty-seven percent of participants reported they are very likely and fifty-eight percent of participants reported they are likely to implement environmental modifications with hearing impaired residents in the future. Fifteen percent of participants reported they are undecided to implement environmental modifications with hearing impaired residents in the future. Overall, the majority of participants reported they are more likely than not to implement environmental modifications with hearing impaired residents in the future. The distribution of responses from all participants is shown in Table 2.
| Question | Strongly Agree | Agree | Neither Agree or Disagree | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| Do you agree that the in-service training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents? | 35% | 46% | 15% | 4% | |
| Do you agree that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids? | 52% | 40% | 8% | ||
| Do you agree that the in-service training adequately prepared them to use assistive listening devices with hearing impaired residents? | 40% | 60% | |||
| Do you agree that the in-service training was personally beneficial overall? | 56% | 40% | 4% |
Table 1: Responses from the second survey on attitudes regarding the in-service training using agree or disagree categories. The grey spaces indicate no responses for that category.
| Question | Strongly Agree | Agree | Neither Agree or Disagree | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| How likely are you implement environmental modifications with hearing impaired residents in the future? | 27% | 58% | 15% | ||
| How likely are you to troubleshoot minor issues with residents’ hearing aids in the future? | 27% | 58% | 15% | ||
| How likely are you to use assistive listening devices with hearing impaired residents in the future? | 32% | 52% | 12% | 4 |
Table 2: Responses from the second survey on attitudes regarding the in-service training using likely or unlikely categories. The grey spaces indicate no responses for that category
For the question “Do you agree that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids (i.e., cleaning and replacing batteries, domes, and wax filters)?”, fifty-two percent of participants reported they strongly agree and forty percent of participants reported they agree that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids. Eight percent of participants reported they strongly disagree that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids. Overall, the majority of participants reported that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids. The distribution of responses from all participants is shown in Table 1.
For the question “How likely are you to troubleshoot minor issues with residents’ hearing aids in the future?”, twenty-seven percent of participants reported they are very likely and fifty-eight percent of participants reported they are likely to troubleshoot minor issues with residents’ hearing aids in the future. Fifteen percent of participants reported that they neither agree nor disagree that they would troubleshoot minor issues with residents’ hearing aids in the future. Overall, the majority of participants reported they are more likely than not to troubleshoot minor issues with residents’ hearing aids in the future. The distribution of responses from all participants is shown in Table 2.
For the question “Do you agree that the in-service training adequately prepared them to use assistive listening devices with hearing impaired residents?”, forty percent of participants reported they strongly agree that the inservice training adequately prepared them to use assistive listening devices with hearing impaired residents. Sixty percent of participants reported they agree that the in-service training adequately prepared them to use assistive listening devices with hearing impaired residents. Overall, the majority of participants reported they agree that the in-service training adequately prepared them to use assistive listening devices with hearing impaired residents. The distribution of responses from all participants is shown in Table 1.
For the question “How likely are you to use assistive listening devices with hearing impaired residents in the future?”, thirty-two percent of participants reported they are very likely and fifty-two percent of participants reported they are likely to use assistive listening devices with hearing impaired residents in the future. Twelve percent of participants reported they are undecided to use assistive listening devices with hearing impaired residents in the future. Four percent of participants reported they are very unlikely to use assistive listening devices with hearing impaired residents in the future. Overall, the majority of participants reported they are more likely than not use assistive listening devices with hearing impaired residents in the future. The distribution of responses from all participants is shown in Table 2.
For the question “Do you agree that the in-service training was personally beneficial overall?”, fifty-six percent of participants reported they strongly agree and forty percent of participants reported they agree that the in-service training was personally beneficial overall. Four percent of participants reported they disagree that the in-service training was personally beneficial overall. Overall, the majority of participants reported they agree that the in-service training was personally beneficial overall. The distribution of responses from all participants is shown in Table 1.
Summary of Results
The respondents in the present study were nursing home staff members with varying degrees of reported experience caring for individuals with hearing impairment. Although these nursing home staff members currently care for residents with hearing impairment, the responses on the pre-survey indicated a need for improvement in training regarding hearing loss, training with hearing aids, and training with assistive listening devices used by residents with hearing loss. Prior to attending the in-service workshop, respondents reported they were as likely as not to have received formal education regarding the care of individuals with hearing impairment. The majority of respondents reported they agree (54%) or strongly agree (20%) that a seminar addressing special considerations for elderly individuals and nursing home residents with hearing impairment would be personally beneficial. When asked if they believe such a seminar would be likely to influence their care of residents with hearing impairment, 80% of respondents reported probably yes (43%) or yes (37%). Sixtyfive percent of respondents reported they would be very likely (34%) or likely (31%) to attend such a seminar if provided free of charge. Following attendance at the in-service training workshop, the majority of respondents reported significant improvement in personal confidence regarding how and when to make appropriate hearing loss and/or amplification referrals, willingness to change a dome or wax filter on a resident’s hearing aid, familiarity with the different hearing aid styles (behind-the-ear, in-the-ear, receiver-in-the ear, etc.), and familiarity with cochlear implants, personal FM systems, sound-field FM systems, TV streamers, and amplified telephones.
Eighty-one percent of respondents reported they agree (46%) or strongly agree (35%) that the in-service training adequately prepared them to implement environmental modifications to improve communication with hearing impaired residents. The majority of respondents reported they are likely (58%) or very likely (27%) to implement environmental modifications in the future. The majority of respondents reported they strongly agree (52%) or agree (40%) that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids, with the majority of respondents reporting they are likely (52%) or very likely (44%) to troubleshoot minor issues with residents’ hearing aids in the future. The majority of respondents reported they agree (60%) or strongly agree (40%) that the in-service training adequately prepared them to use assistive listening devices with hearing impaired residents, with the majority of respondents reporting they are likely (52%) or very likely (32%) to use assistive listening devices with hearing impaired residents in the future. The majority of respondents reported they strongly agree (56%) or agree (40%) that the in-service training was personally beneficial overall.
CONCLUSIONS
The results of the present study indicated that most nursing home staff personnel are not knowledgeable when it comes to hearing health care and overall benefitted from in-service training. While most participants indicated benefit from the training, a small percentage indicated that they felt the in-service was not beneficial in certain areas. Four percent of participants indicated that they strongly disagreed for question “Do you agree that the inservice training adequately prepared them to use environmental modifications to improve communication with hearing impaired residents?” It may be that the participants felt that the in-service did not cover this topic area adequately and future in-services should expand this topic area. Another suggestion to increase preparedness among nursing home staff members would be to implement role playing during the in-service to simulate common communication issues found in nursing homes where environmental modification could be made.
Eight percent of participants indicated that they strongly disagreed for question “Do you agree that the in-service training adequately prepared them to troubleshoot minor issues with residents’ hearing aids?” A handson portion added to future in-service trainings could help prepare nursing home staff members in this topic area where troubleshooting hearing aids may be difficult to understand when information is presented by audition only. For the question “How likely are you to use assistive listening devices with hearing impaired residents in the future?”, four percent of participants indicated that they were very unlikely to use assistive listening devices with hearing impaired residents in the future. A possible explanation for this is that the participants may have felt unprepared without actually getting trained on those type of devices. An expansion of the in-service could include a hands-on training portion on the most common assistive listening devices that could be used in a nursing home. Four percent of participants indicated that they disagreed for question “Do you agree that the in-service training was personally beneficial overall?” The reason for this could be the lack of hands-on training and the feeling that some of the topic areas should be expanded on during the in-service.
While the present study did not address a hands-on training, it would most likely be beneficial to nursing home staff members to be trained on proper insertion and removal of hearing aids, how to perform a listening check, how to replace the hearing aid battery, hearing aid maintenance, basic hearing aid troubleshooting, and the appropriate protocol to follow if a resident’s hearing aid is not functioning properly. A future study should address adding a hands-on component to the training as well as follow-up surveys to assess whether the training for the nursing home staff carries over into practice or is lost over time.
Based on data collected in the present study, nursing home staff member training should include causes of hearing loss, effects of hearing loss on quality of life, types and components of hearing aids and assistive listening devices, basic troubleshooting and maintenance of hearing aids, clear communication strategies, and listening environment modifications for the hearing impaired. This conclusion was reached based on the lack of knowledge of the nursing home staff members found during the initial survey prior to the in-service training. In an effort to facilitate the best quality of life for nursing home residents, providing hearing aid and assistive listening device orientation to each new nursing home staff member is recommended to ensure that hearing impaired residents are able to communicate comfortably and confidently with their caregivers. Based on the results of this study, the training was considered effective.
REFERENCES
- U.S. Census Bureau. 65+ in the United States: 2010. U.S. Government Printing Office, Washington, DC. 2014; 23-212.
- Burkhalter CL, Allen RS, Skaar DC, Crittenden J, Burgio LD. Examining the effectiveness of traditional audiological assessments for nursing home residents with dementia-related behaviors. J Am Acad Audiol. 2009; 20: 529-538.
- Jenkins M. Delivering effective service to nursing homes. Hearing Instruments. 1995; 18.
- Busacco D. Cost-effective hearing health care services in long term care facilities. Audiology Online. 2009.
- Weinstein B, Amsel L. Hearing loss and senile dementia in the institutionalized elderly. Clinical Gerontologist. 1986; 4: 3-15.
- Mulrow CD, Aguilar C, Endicott JE, Tuley MR, Velez R, et al. Quality-of-life changes and hearing impairment. Ann Intern Med. 1990; 113: 188-194.
- Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, et al. The impact of hearing loss on quality of life in older adults. Gerontologist. 2003; 43: 661-668.
- Huang Q, Tang J. Age-related hearing loss or presbycusis. European Archives of Oto-Rhino-Laryngology. 2010; 267: 1179-191.
- Lesner SA. Candidacy and management of assistive listening devices: special needs of the elderly. Int J Audiol. 2003; 42: 68-76.
- Cohen-Mansfield J, Taylor JW. Hearing aid use in nursing homes, part 2: barriers to effective utilization of hearing aids. J Am Med Dir Assoc. 2004; 5: 289-296.