Low-Grade Endometrial Stromal Sarcoma Which Relapsed a Month after Transcervical Resection as Fertility-sparing Surgery and Diagnosed with Laparoscopic Hysterectomy
Takeda T*1,2 , Tamada Y3, Matoba Y 1,2, Saotome K1, Makabe T1,2
1 Department of Obstetrics and Gynecology, Tachikawa Hospital, Tachikawa, Tokyo, Japan
2 Department of Obstetrics and Gynecology, Keio University School of Medicine, Shinjyuku, Tokyo, Japan
3 Department of Gynecology, Jyoban Hospital, Tokiwa Foundation, Iwaki, Fukushima, Japan
ABSTRACT
We report a case of 36-year-old female who was treated for a submucosal tumor. She received transcervical resection for submucosal tumor and it was diagnosed as an endometrial stromal nodule (ESN) with muscle differentiation which showed no malignant potential. Fertility-sparing surgery was completed, however, the tumor relapsed a month after surgery. Laparoscopic hysterectomy was performed for diagnosis and treatment. Pathological finding from removed uterus showed low-grade endometrial stromal sarcoma (LGESS) with smooth muscle differentiation. This is an instructive case that endometrial stromal tumors are difficult to diagnose since it cannot be examined fully in fragmented species and low-grade endometrial stromal sarcoma can rapidly develop within a month. Early relapse of the endometrial stromal tumor may have a malignant potential and post-surgical follow-up after fertility-sparing surgery is necessary. Finally, hysterectomy is needed to diagnose the malignant potential of endometrial stromal tumors.
Key Words: Fertility sparing surgery, Laparoscopic hysterectomy, Low grade endometrial stromal sarcoma, Transcervical resection
INTRODUCTION
Endometrial stromal nodule (ESN) is a benign endometrial stromal tumor which has a well–circumscribed margin and is composed of cells that resemble proliferative-phase endometrial stroma, and it is a relatively rare neoplasm. Low-grade endometrial stromal sarcoma (LGESS) is a malignant tumor displaying infiltrative growth into the myometrium. It represents less than 1% of all uterine malignancies. It occurs at a wide range with a mean age of 52 years, however, the patients tend to be younger than those with other uterine sarcomas [1].
Endometrial stromal tumor can display admixture of smooth muscle differentiation, fibromyxoid, sex cord-like differentiation and many other variant. Endometrial stromal tumor with smooth muscle differentiation, previously called mixed endometrial stromal and smooth muscle cell tumor (MSST), is the most often seen valiant and classified into benign, malignant, and low-grade malignancy, determined by the most malignant component among pathological findings of a tumor [1-3].
Endometrial stromal tumors are often diagnosed as leiomyoma preoperatively because of its difficulty in diagnosing with MRI. Additionally, diagnosis of ESN and LGESS is difficult especially in tumor resection because it depends on the stromal invasion. We report a case diagnosed as LGESS with smooth muscle differentiation which could not detect the malignancy and resected with hysteroscopy as a fertility-sparing surgery, however relapsed within a month and diagnosed with laparoscopic hysterectomy.
CASE PRESENTATION
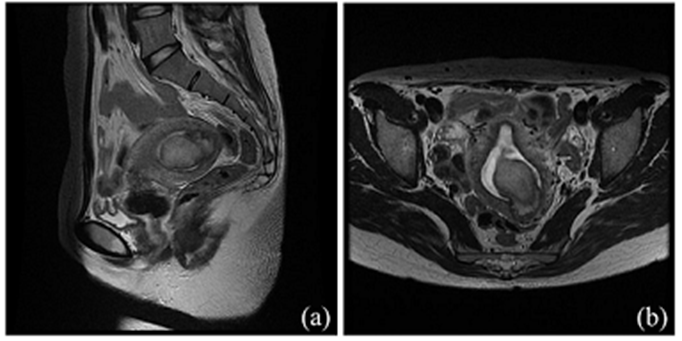
A 36-year-old woman who had severe anemia (hemoglobin 4.9 g/dL) and a 3 cm submucosal myoma was referred to us from another gynecological outpatient clinic. She was a married woman and had two times experiences of vaginal delivery. It was definite that her submucosal tumor caused hypermenorrhea and severe anemia. Her menstrual cycle was normal, and her past history was not significant. On examination, her vital signs were stable and vaginal examination revealed a goose-egg-sized uterus. In investigations, her hematological and biochemical profile was normal except for hemoglobin data (5.8 g/dL). Transvaginal ultrasonography (TVUS) showed a submucosal tumor measuring a maximum of 3.8 cm in the uterus. Pelvic magnetic resonance imaging (MRI) also showed the uterine tumor as a 4 cm-sized submucosal fibroid protruding from the uterine fundus to the endometrial cavity (Figure 1). Cervical and endometrial cytology showed negative for intraepithelial lesion or malignancy (NILM) and negative respectively. Tumor markers like CA125, LDH, and CA19-9 were measured and were found to be normal.
Figure 1: Pre-operative image of pelvic MRI
(a) sagittal image. A 40mm-sized submucosal fibroid in the uterus. (b) horizontal image. It looked invasive in some parts and cannot deny the possibility of low-grade endometrial stromal sarcoma.After the improvement of her hemoglobin data by the therapy of anemia, we performed transcervical resection (TCR) of the tumor as a fertility-sparing surgery. The tumor had a stalk and about 100 % protruding from the uterine fundus in hysteroscopy. The tumor was seemed to be resected completely in the intrauterine cavity, however, it was uncertain that the deepest lesion of the tumor could be fully removed. (Figure 2).
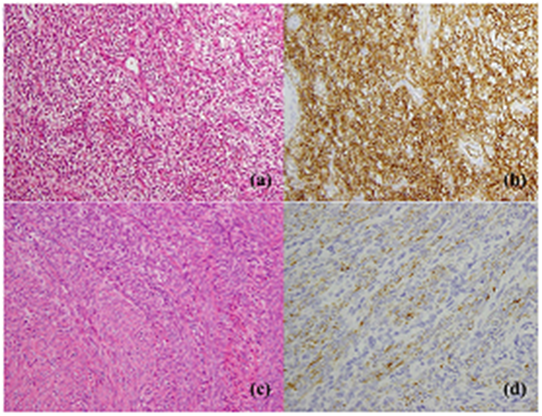
Pathological findings of the resected tumor were suggestive of ESN with muscle differentiation. There was a proliferation of endometrial stromal cells and nodular differentiation of smooth muscle cells with no necrotic tissue. Proliferative cells were positive for CD10 and nodular parts were positive for desmin. The tumor seemed to be invasive in some parts, but the invasion was less than 3mm. ESN with smooth muscle differentiation was most likely and there was no evidence of malignancy in TCR specimens (Figure 3).
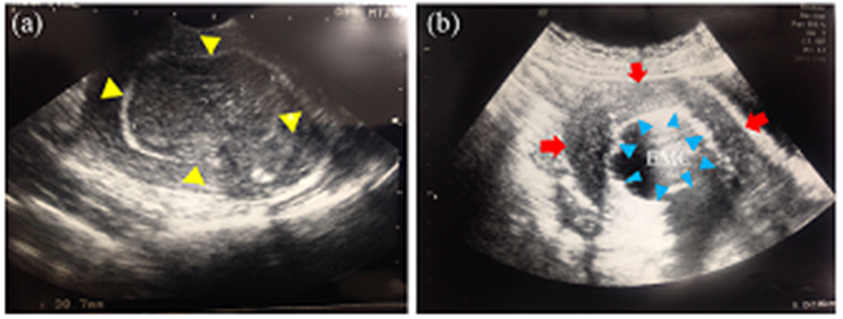
Figure 2: Ultrasonographical findings
(a) transvaginal ultrasonography before surgery showed 38mm-sized submucosal tumor. (yellow arrowhead) (b) post-operative transabdominal hysterosonography. Blue arrowhead showed uterine endometrium and endometrial cavity was full with saline after tumor resection. (Red arrow showed uterine myometrium). EMC: endometrial cavityFigure 3: Microscopic findings ((a)(b): x100, (c)(d): x200)
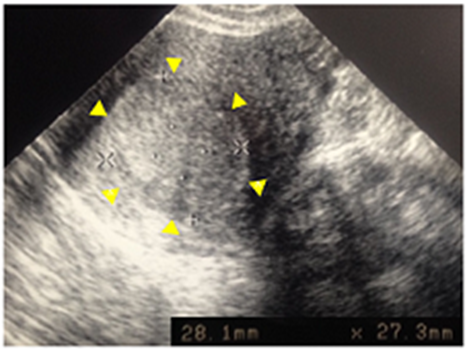
Her postoperative course was uneventful. A month after the fertility-sparing surgery a 28mm-sized tumor recurred in the uterus (Figure 4). We thought that the tumor could be LGESS on the basis of the previous pathological findings and also on the fact that it recurred rapidly. After having checked with a computed tomography (CT) scan that there was no metastatic finding, we recommended her to have a hysterectomy due to the possibility of a malignant tumor.
Figure 4: Transvaginal ultrasonography a month after fertility-sparing surgery.
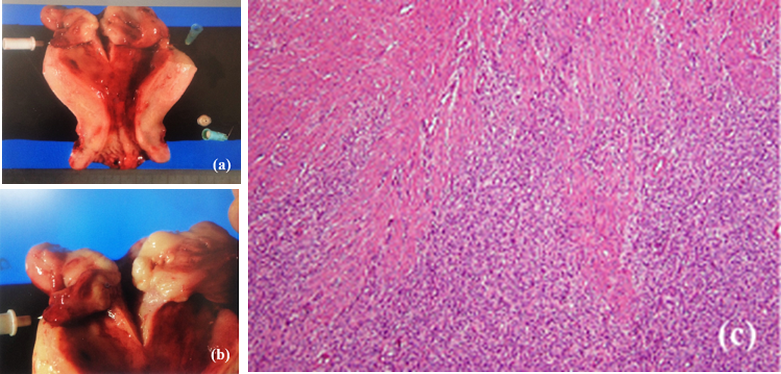
Ultrasonography showed 28mm-sized relapsed submucosal tumor. (yellow arrowhead)We performed a laparoscopic hysterectomy. Both her ovaries looked normal and there was no metastatic lesion in her abdominal cavity. Intrauterine mass was a 3cm-sized tumor and it infiltrated to myometrium macroscopically. The pathological diagnosis of the removed uterus was LGESS with smooth muscle differentiation and the post-surgical stage was stage IA (Figure 5). She is now followed up without recurrence.
Figure 5: Macro and microscopic findings
(a) tumor was developed from the fundus of uterus. (b) tumor looked invasive macroscopically. (c) invasive lesion of tumor into surroundings (HE stain). (×100)DISCUSSION
Endometrial stromal tumor with smooth muscle differentiation is the variant of endometrial stromal tumor that most often seen according to WHO Classification of Tumors of Female Reproductive Organs (Fourth Edition) [1]. It was previously called mixed endometrial stromal and smooth muscle cell tumor according to WHO Classification of Tumors of Female Genital Organs (Third Edition) [2] and classified into benign, low-grade malignancy, and malignant, based on the most malignant component by the general rules for clinical and pathological management of uterine corpus cancer edited by Japan Society of Obstetrics and Gynecology [3]. A benign endometrial stromal tumor is referred to as endometrial stromal nodule (ESN), while the low-grade malignant tumor is referred to as low-grade endometrial stromal sarcoma (LGESS). A difference between ESN and LGESS depends on the stromal invasion. While ESN shows exclusive tumor growth, LGESS grows invasively [1]. Both tumors have similar findings in high power magnification field and a number of mitosis in each tumor is not decided on their differential diagnosis. Therefore, it is difficult to diagnose these tumors and hysterectomy is necessary to confirm the boundary of a tumor for definitive diagnosis of malignancy.
Immunohistochemical staining is not necessary but helpful for its diagnosis. Endometrial stromal components are largely positive for CD10, and smooth muscle components are mostly positive for desmin, α-smooth muscle actin (SMA), and vimentin [4-6]. CD10 and desmin were positive in our case, which supported the diagnosis. Also, these immunochemical staining can be useful for differential diagnosis from low-grade ESS to variant smooth muscle tumors such as cellular leiomyoma.
An appropriate surgery would be hysterectomy and bilateral salpingo-oophorectomy in this LGESS case, however, it was difficult to diagnose LGESS before surgery and also after TCR because the surgical margin is unclear and surgical tissues receive heat denaturation. Also, the way of hysterectomy in the case of LGESS should be abdominal hysterectomy, however we chose laparoscopic hysterectomy for minimally invasive surgery because it is uncertain that the tumor had a malignant potential. Finally, bilateral salpingo-oophorectomy was not performed after the final diagnosis of LGESS because of the patient’s refusal.
Several reports showed the results of fertility-sparing surgery for LGESS [7-9]. The latest report of fertility-sparing surgery for LGESS concluded that fertility-sparing surgery may be considered for young patients with stage IA LGESS who wish to preserve the fertility [10]. Among these reports, the shortest recurrence periods were three months. This case showed one month for recurrence and to the best of our knowledge, this is the shortest recurrence period ever reported. Therefore, close follow-up is recommended if the tumor is diagnosed as LGESS and also even ESN after fertility-sparing surgery.
ACKNOWLEDGMENT
I am deeply grateful to Dr. Tamada for giving insightful comments and suggestions.
REFERENCES
- Kurman RJ, Carcangiu ML, Herrington CS., Young RH. WHO Classification of Tumours of Female Reproductive Organs. IARC WHO Classification of Tumours. 4th ed. Lyon: International Agency for Research on Cancer. 2014.
- Tavassoéli FA, Devilee P. Pathology and Genetics Tumours of the Breast and Female Genital Organs. IARC WHO Classification of Tumours. 3rd ed. Lyon: International Agency for Reesarch on Cancer. 2003.
- Katabuchi H, Mikami M. The general rules for clinical and pathological management of uterine corpus cancer. 3rd ed. Tokyo, Kanehara; 2012.
- Chu PG, Arber DA, Weiss LM, Chang KL. Utility of CD10 in distinguishing between endometrial stromal sarcoma and uterine smooth muscle tumors: an immunohistochemical comparison of 34 cases. Mod Pathol. 2001; 14: 465-4671.
- Coganow M, Das BM, Chen E, Crestanello JA. Single-stage resection of a mixed endometrial stromal sarcoma and smooth muscle tumor with intracardiac and pulmonary extension. Ann Thorac Surg. 2006; 82: 1517-1519.
- Shintaku M, Hashimoto H. Mixed endometrial stromal and smooth muscle tumor: report of a case with focal anaplasia and early postoperative lung metastasis. Pathol Int. 2013; 63: 214-219.
- Morimoto A, Tsubamoto H, Inoue K, Ikeda Y, Hirota S. Fatal case of multiple recurrences of endometrial stromal sarcoma after fertility-sparing management. J Obstet Gynaecol Res. 2015; 41: 162-166.
- Maeda O, Moritani S, Ichihara S, Inoue T, Ishihara Y, et al. Long-term survival in low-grade endometrial stromal sarcoma with childbirth and multidisciplinary treatment: a case report. J Med Case Rep. 2015; 9: 233.
- Laurelli G, Falcone F, Scaffa C, Messalli EM, Del Giudice M, et al. Fertility-sparing management of low-grade endometrial stromal sarcoma: analysis of an institutional series and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2015; 195: 61-66.
- Xie W, Cao D, Yang J, Jiang X, Shen K, et al. Fertility-sparing surgery for patients with low-grade endometrial stromal sarcoma. Oncotarget. 2016.
Corresponding author: Takashi Takeda, M.D., Department of Obstetrics and Gynecology, Tachikawa Hospital, Tachikawa, Tokyo, Japan. Department of Obstetrics and Gynecology, Keio University School of Medicine, Shinjyuku-ku, Tokyo, Japan. Tel: (+81)-3-3353-1211.
Received: Nov 23, 2016; Accepted: Dec 17, 2016; Published: Dec 20, 2016
CC: This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.
Cite as: Takeda T, Tamada Y, Matoba Y, Saotome K, Makabe T. Low-Grade Endometrial Stromal Sarcoma Which Relapsed a Month after Transcervical Resection as Fertility-sparing Surgery and Diagnosed with Laparoscopic Hysterectomy. J Gynecol Fertil. 2016; 1: 1-7.