Journal of Communication Disorders and Assistive Technology
ISSN: 2576-3997
Early Intervention Case Study: Bone-Anchored Hearing Aid (BAHA) Softband Fitting in Treacher Collins Syndrome
Diane Davis1 and Yula C. Serpanos*
1Department of Communication Sciences and Disorders, Adelphi University, Garden City, NY, 11530-0701
KEYWORDS
Bone-anchored hearing aid, Treacher collins syndrome, Hearing loss, Implantation, Softband fitting
ABBREVIATIONS
BAHA: Bone-Anchored Hearing Aid
TCS: Treacher Collins Syndrome
CHL: Conductive Hearing Loss
BC: Bone conduction
ABSTRACT
This retrospective case study reports on the successful auditory and language outcomes following bone-anchored hearing aid (BAHA) Softband fitting in a child with Treacher Collins syndrome (TCS) and moderately severe conductive hearing loss (CHL) resulting from bilateral aural atresia. Information is presented from birth to age 3 years. The timeframe of assessment and remediation services met 1-2-3-month early intervention target guidelines. The child received the medical intervention, a hearing diagnosis, and a remediation plan for BAHA Softband fitting along with family-centered early intervention support services, including speech and language, within 3 weeks following birth. The BAHA Softband was fitted at age 2 months. Developmental milestones for language comprehension were met by age 7 months. The timeline of assessments, interventions, and outcomes, in this case, the study illustrated a collaborative team management approach involving medical practitioners, audiologists, speech-language pathologists, early intervention coordinators, family service providers, educators, and parents, aimed toward the development of appropriate communicative milestones in children with TCS and CHL.
INTRODUCTION
Treacher Collins syndrome (TCS) occurs in 1 of 50,000 newborns and results from mutations in the TCOF1, POLR1C,or POLR1D gene affecting the tissues and bone development of the head and face. The disorder is commonly characterized by variable craniofacial malformations present at birth often involving the eyes, facial bones, mandible, and palate, as well as defects of the outer and middle ears. Rare features include microcephaly, limb anomalies, renal, cardiac, and intellectual disorders [1-3]. The management of TCS requires a multidisciplinary approach with varied short and long-term interventions over the lifespan that may include tracheotomy, craniofacial reconstruction, orthodontic treatment, hearing amplification, and speech therapy [4,5]. The most common ear anomalies in TCS are bilateral, and include abnormal positioning of the pinna, microtia, external auditory canal atresia, middle ear cavity deformation, and malformation or absence of the ossicles. Unilateral or bilateral hearing loss is prevalent and approximately half of those with TCS present with bilateral conductive hearing loss (CHL) of varied degree from mild to severe according to the extent of the otologic involvement. The hearing loss can be remediated with amplification and aural rehabilitation services to mitigate speech and language delays and to enhance communication skills, particularly in children [6-9].
Microtia and ear canal atresia are very frequent features in TCS occurring in ~70% of individuals [10] The outer ear anomalies in TCS pose a challenge in fitting traditional air conduction hearing aids and therefore alternative management strategies using bone conduction (BC) amplification systems is considered for those with CHL. BC amplification devices bypass the outer ear and convert sound energy into bone vibrations against the skull that directly stimulate the cochlea. Conventional BC hearing aids consist of a bone vibrator held firmly in place against the overlying skin of the mastoid using a hard band or eyeglasses [11]. Because the bone vibrator requires high pressure and consistent contact against the skull to stimulate effective mechanical vibration, the devices can be uncomfortable when worn long term, particularly in young children. Adverse reactions using conventional BC hearing aids include headaches, skin irritations, pressure sores, skull depressions, and poor cosmetic appeal. Further, the difficulty in maintaining stability in the placement of the vibrator over the mastoid bone can lead to poor sound quality [12,13].
Surgically implanted BC amplification systems, known generically as bone-anchored hearing aids (BAHA), mitigate many of the issues with conventional BC amplification. The BAHA is composed of internal and external portions; a titanium osseointegrated implant is surgically embedded in the cortex of the temporoparietal bone behind and above the outer ear and connects to an external sound processor either directly via a percutaneous abutment, or magnetically in transcutaneous systems. Sounds that enter the external sound processor are converted into vibrations through the implant and surrounding bone and then transferred to the cochlea in the inner ear [14-16]. A delayed fitting of surgically implanted BAHA is recommended in young children to allow development of cortical bone for better osteointegration with the implant. The minimum fitting age for a BAHA system is ≥ 5 years in the United States and Canada whereas cortical thickness (≥ 3 mm) is considered in France [16]. An international consensus developed by BAHA clinics in Europe, Canada, and the United States reported that it is inadvisable to perform BAHA implantation before the age of 2 to 3 years [11]. However, early intervention of children with hearing loss by age 6 months is considered optimal to achieve communication and linguistic competence [17]. The BAHA device can be worn non-surgically attached to a soft headband in early childhood instead of or until surgical BAHA is appropriate [11,16]. In this configuration known as the BAHA Softband, the BAHA sound processor is connected via a plastic disc to an elastic band fastened around the head [11].
Few studies have been published demonstrating hearing and communication benefit using the BAHA Softband in children with TCS and CHL from congenital bilateral aural atresia but have supported the device as a viable alternative treatment without or prior to surgical BAHA. Verhagen et al. [18] reported on 12 children, 7 with TCS, presenting with bilateral congenital aural atresia and CHL. These children were fitted with unilateral or bilateral BAHA Softband at an average age of 2 years 3 months and compared to a control group of 8 children without TCS remediated with conventional BC amplification. The amplification with the BAHA Softband was found comparable in performance but reported as more comfortable than wearing the steel head band of the BC device. Nicholson et al. [19] conducted a retrospective review of 25 children with craniofacial disorders and bilateral CHL fitted with a unilateral BAHA Softband device. Eight of these children presented with TCS and ranged in age from 1.5 to 14 years, but information was not provided on the fitting age with the BAHA Softband. The outcomes verified the benefit of the BAHA Softband in providing effective audibility across the speech spectrum (for octave frequencies 500 through 4000 Hz) for these children [19].
There are limited accounts of speech and language performance following BAHA Softband fitting in children with TCS presenting with CHL from bilateral aural atresia. Verhagen et al. [18] reported the receptive language outcomes for 5 of a larger group of 12 children presenting with bilateral congenital aural atresia and CHL but did not specify those presenting with TCS. The language development results reported for these children fitted with the BAHA Soft-band were found typical to peers with good hearing. Polanski et al. [20] reported on the hearing and speech outcomes in a child with TCS and bilateral aural atresia fitted a BAHA Softband at age 2 years and 10 months following poor acceptance of a BC device arising from discomfort due to skull compression. One month after the activation of the BAHA system, parental questionnaires identified improvements in the child’s communicative intent and listening skills, including sound localization, detection, and recognition of verbal sounds.
This retrospective case study reports on the audiologic and speech and language outcomes in a child with TCS and bilateral aural atresia fitted with BAHA Softband devices and followed from the age of 3 weeks to 34 months. This case report provides two unique perspectives from other information in the current literature. First, it provides a timeline of assessment and intervention outcomes and services initiated in a child with TCS and bilateral aural atresia remediated with the BAHA Softband less than 3 months of age. Further, information from this case study illustrates the effectiveness of early intervention and a birth to age 3-year timeframe of a collaborative team management approach involving medical, audiology, speech-language pathology, and family-centered services that are geared toward early communication development in a child with TCS and CHL.
History
The child is a White female with a diagnosis of TCS, who was evaluated and treated in the northeast region of the United States in the past few years. She was diagnosed with congenital clefts of the hard and soft palate, micrognathia, cardiovascular disorder (patent ductus arteriosus and patent foramen ovale) and bilateral aural atresia. Following birth in a hospital setting, the child was admitted to the neonatal intensive care unit (NICU). A tracheostomy was performed, and a nasogastric tube was inserted for feeding. She was discharged from the hospital at age 2 weeks. The cardiovascular disorder was monitored by a cardiologist. Surgical repair of the soft and hard palate occurred at the age of 16 months. The tracheostomy tube was removed at 20 months. This case study involved an examination of pre-collected and de-identified data and therefore ethical review and approval including patient consent were waived by the institutional review boards of the case site affiliations.
Assessment and Management Timeline
Birth to 7 months
An air conduction newborn hearing screening was not performed in the NICU due to the bilateral aural atresia. The child returned to the birth hospital at the age of 3 weeks for outpatient diagnostic BC auditory brainstem response (ABR) testing performed by an audiologist. The BC ABR click, 500 Hz tone burst, and 2000 Hz tone burst threshold responses were recorded bilaterally at 20 to 30 dB nHL, consistent with normal BC hearing sensitivity in both ears [21,22). Bilateral CHL was considered probable due to the bilateral aural atresia. At this time, a unilateral BAHA Softband device was recommended. Referrals were made for consultation with an otorhinolaryngologist, further audiologic assessment, and early intervention (EI) services. In accordance with federal and state-approved practices, EI services were provided under the Individualized Family Service Plan (IFSP), which is a team-based, family-centered approach for developing tailored treatment plans for eligible children from birth to age 3 years [23]. The IFSP included the assignment of a service coordinator to plan and coordinate services that included audiology, speech and language, and assistive technology. A referral was made by the EI Official Designee to an audiologist at a state approved evaluation center for further audiologic assessment, management, and assistive technology services.
Speech and language services were provided in the home twice weekly for 45-minute sessions by a licensed speech-language pathologist through the EI program. Evaluations using the Preschool Language Scale ([PLS]; editions 4 [PLS-4] and 5 [PLS-5] [24,25] were performed at 1 month of age and thereafter at 6-month intervals to monitor progress. Data were available for ages 1, 7, 19, and 25 months and are presented in Table 1. Standard scores for auditory comprehension, expressive communication and total language were outside the normal range at the age of 1 month.
At the age of 2 months the Cochlear Baha® BP100 Softband was dispensed for the right ear. The instrument was tolerated well. Aided sound field testing was performed using unconditioned behavioral observation audiometry (BOA) and responses were obtained at 40 to 55 dB HL from 500 to 4000 Hz. The aided responses were within guidelines of expected behavioral auditory response levels at this age [26] suggesting that the device was providing adequate benefit. The family was counseled on device use and maintenance. The Early Listening Function (ELF) instrument was provided to the parents to determine the functional use of hearing with amplification. The ELF was developed as a tool for audiologists and early interventionists working with parents and caregivers of infants and toddlers (4 months to 3 years) with hearing loss to engage parental involvement, obtain an estimation of benefit with amplification, and to track improvements in auditory development [27]. In this case study, the ELF was reviewed by the audiologist, speech-language pathologist, and other EI team members with the parents at each visit for information on performance with the device. Detailed information on the ELF outcomes was not available but is outlined below where applicable.
Aided BOA testing at age 5 and 7 months replicated performance at age 2 months supporting age-appropriate auditory responses and appropriate benefit with the device. Speech and language assessment at age 7 months (Table 1) showed the auditory comprehension standard score within normal limits. Expressive communication and total language standard scores improved from performance at age 1 month but continued to be outside the normal range of development.
| Variable | PLS-4 Standard Score | PLS-4 Standard Score | PLS-5 Standard Score | PLS-5 Standard Score |
|---|---|---|---|---|
| Age (months) | 1 | 7 | 19 | 25 |
| PLS | ||||
| Auditory Comprehension | 75 | 88 | 92 | 100 |
| Expressive Communication | 62 | 77 | 78 | 77 |
| Total Language | 63 | 81 | 84 | 88 |
Note: Speech and language assessments were obtained using the Preschool Language Scale (PLS) editions 4 (PLS-4) and 5 (PLS-5).
Table 1: Speech and language assessment outcomes from ages 1 month to 25 months
8 to 13 months
At the age of 8 months, reliable unaided air conduction and BC conditioned audiometry using visual reinforcement audiometry (VRA) was conducted in the soundfield. Unaided air conduction thresholds responses were recorded at 65 to 75 dB HL and BC thresholds were 15 to 20 dB HL at 500 to 4000 Hz supporting a moderately-severe to severe [28] CHL for at least the better ear (Table 2). The performance of the BAHA Softband instrument was evaluated in the soundfield using VRA audiometry at the age of 9 months. Aided thresholds were obtained at 25 to 30 dB HL supporting good benefit with the instrument (Figure 1). The aided thresholds were replicated at 12 and 13 months.
| Test | Age (months) | Transducer | Ear | Hearing Thresholds (dB HL) by Frequency | |||
|---|---|---|---|---|---|---|---|
| 500 Hz | 1000 Hz | 2000 Hz | 4000 Hz | ||||
| VRA | 8 | speaker | - | 65 | 70 | 65 | 75 |
| bone oscillator | - | 15 | 15 | 20 | 20 | ||
| VRA | 16 | speaker | - | 65 | 60 | 60 | 70 |
| VRA | 20 | headphone | R | 60 | 65 | 60 | 65 |
| headphone | L | 65 | 65 | 65 | 65 | ||
| bone oscillator | - | 20 | 15 | 25 | 20 | ||
| CPA | 25 | headphone | R | 65 | 65 | 65 | 60 |
| headphone | L | 65 | 65 | 60 | 60 | ||
Note: VRA = visual reinforcement audiometry; CPA = conditioned play audiometry
Table 2: Unaided serial behavioral testing and outcomes
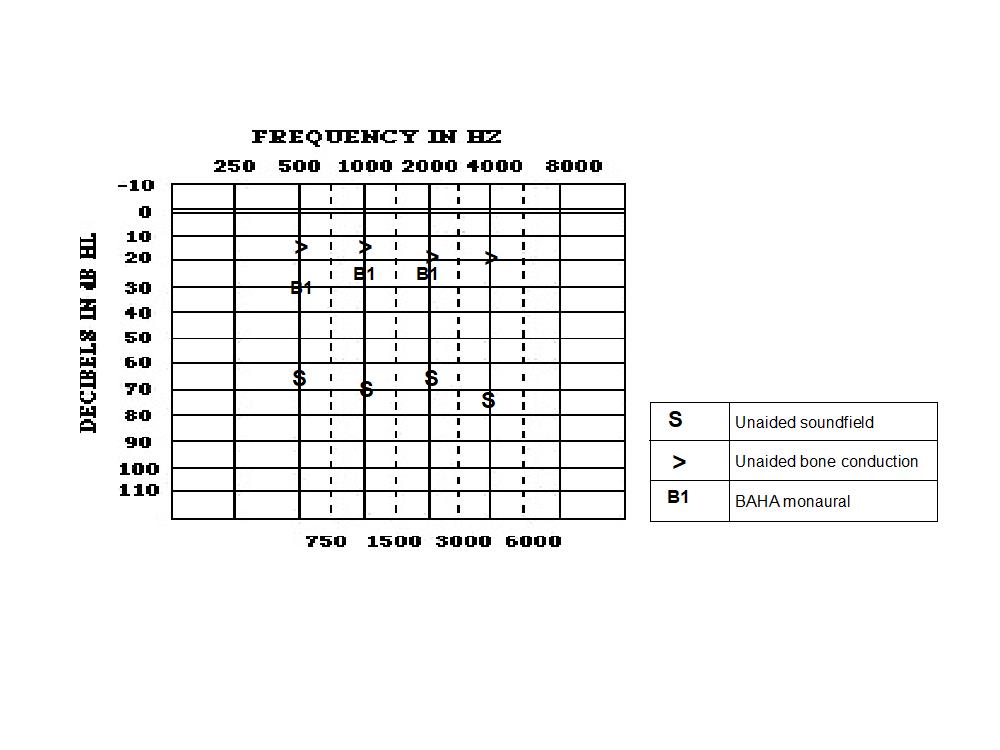
Note: Unaided air (soundfield) and bone conduction hearing thresholds at 8 months; aided monaural BAHA hearing thresholds at 9 months.
Figure 1: Unaided and aided monaural BAHA hearing thresholds
16 to 19 months
Follow up hearing assessments were performed using VRA audiometry at 16, 17, and 19 months of age. Unaided hearing thresholds in soundfield (60 to 70 dB HL) were consistent with those measured at 8 months (Table 2). Aided thresholds with the BAHA Softband (20 to 30 dB HL) supported previous findings at 9, 12, and 13 months of age. Speech and language assessment at 19 months showed the standard scores for auditory comprehension and total language within normal limits. Expressive communication scores remained outside the normal range (Table 1).
20 to 27 months
At 20 months, reliable ear-specific unaided hearing threshold information was obtained with VRA audiometry under headphones. Air conduction thresholds were obtained at moderately severe levels (60 to 65 dB HL) bilaterally, consistent with previous outcomes in soundfield (Table 2). The child’s parents reported that the process was started for enrollment in a family infant program at a school for the Deaf. The program provided music classes and individual family sessions with the child and a multidisciplinary team member. In the family infant program, strat- egies were provided for the parent and child to promote auditory, speech, language, and cognitive development. A recommendation was made for binaural BAHA Softband instruments and a frequency modulated (FM) system. At the parent’s request an audio adapter was ordered and delivered to connect the BAHA Softband with a tablet computer.
At the age of 25 months a Phonak FM system with an Easylink transmitter and MLXi receiver was fitted to the BAHA Softband device. Conditioned play audiometry (CPA) was performed at 25 months to evaluate unaided and aided hearing. Unaided air conduction thresholds confirmed moderately severe levels (60 to 65 dB HL) bilaterally, consistent with previous outcomes under headphones (Table 2). CPA was used to measure aided monaural BAHA Softband thresholds. Aided thresholds were obtained at 15 to 30 dB HL from 500 to 4000 Hz, further supporting appropriate amplification with the device. An improvement of 15 dB HL at 500 Hz was noted in aided performance compared at age 9 months (Figures 1 and 2), however this may be attributed to maturational differences in testing. Speech and language assessment showed an improvement in the standard scores for auditory comprehension and total language at 25 months, while expressive communication standard scores remained outside the normal range (Table 1)
At 27 months the Cochlear BAHA BP 100 Softband was fitted for the left ear to initiate a binaural BAHA fitting. A comparison of monaural and binaural aided testing using CPA revealed slightly improved functional gain (5 dB) with binaural amplification, however this may be due to maturational or retest differences (Figure 2).
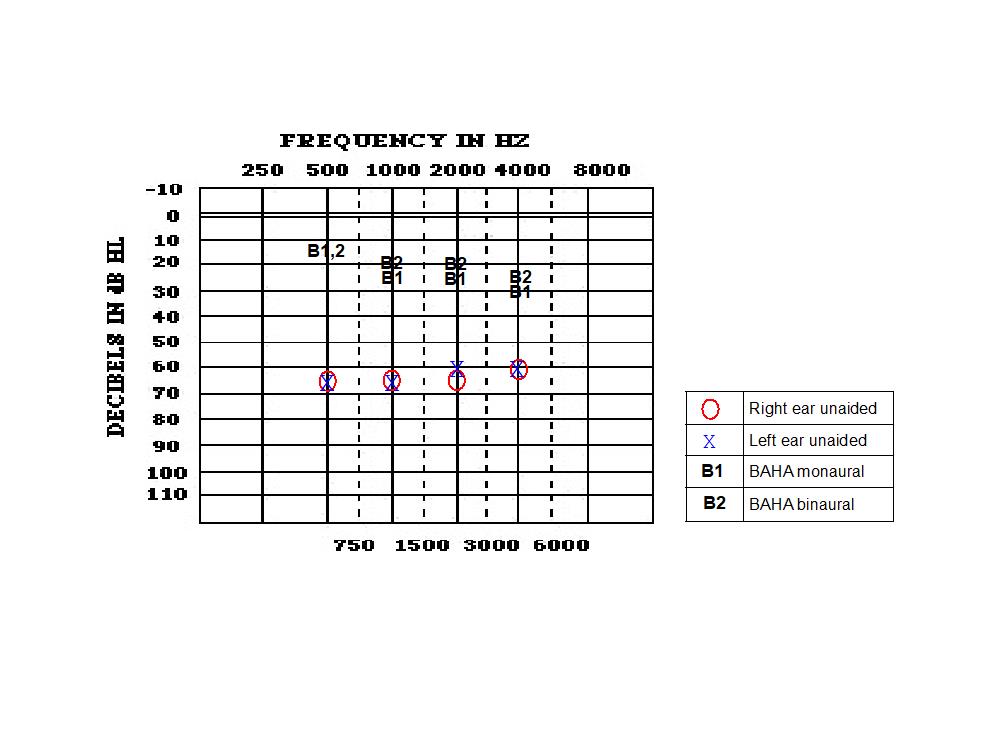
Note: Unaided hearing thresholds at 25 months; aided monaural BAHA hearing thresholds at 25 and 27 months; aided binaural BAHA thresholds at 27 and 34 months.
Figure 2: Unaided and aided monaural and binaural BAHA hearing thresholds
34 months
Aided testing further confirmed the benefit derived from binaural BAHA Softband instruments at the age of 34 months, supporting the outcomes at 27 months (Figure 2). Transition from the EI program occurred at the age of 34 months and the child was referred for further services through the state-approved special education system.
DISCUSSION
This case report highlighted some of the unique considerations for the successful aural habilitation of a child with TCS and CHL from bilateral aural atresia using BAHA Softband, as discussed below.
Amplification Assessment and Verification
The preferred amplification verification procedure using real-ear probe microphone measures is not possible us- ing BC instruments [29]. In the presented case study, aided performance using the BAHA Softband instruments was verified with soundfield audiograms at the initial fitting age of 2 months and re-evaluated every few months. Parental input from the ELF was obtained at each visit providing further verification of amplification. The binaural BAHA Softband fitting initiated at age 27 months demonstrated aided thresholds at 15 to 25 dB HL supporting appropriate benefit [30]. Functional gain outcomes were similar comparing the monaural (30 to 50 dB HL) and binaural BAHA Softband fitting (35 to 50 dB HL; Figure 2).
Pediatric amplification practice guidelines recommend binaural amplification fitting in bilateral hearing loss unless contraindicated [29]. In most patients with bilateral hearing loss, binaural amplification maximizes the advantages of binaural hearing which include: the enhancement of sound intensity; improvement in sound localization; and better speech intelligibility in poor listening conditions such as in background noise and reverberation. In addition, a monaural amplification fitting in bilateral hearing loss may lead to auditory deprivation effects in the unaided ear [31]. Bilateral BAHA fitting in children with bilateral hearing loss has shown improved sound localization and speech recognition in noise [32] and subjective reports of better hearing quality and spatial hearing [33]. Therefore, fitting binaural BAHA devices is considered the best option for those with bilateral hearing loss who qualify for BC systems [11].
Amplification Assessment and Verification
In this case study an FM system was coupled to the BAHA Softband at around age 2 years, when the child began educational services. Pediatric amplification guidelines recommend that all children with hearing loss should be considered candidates for FM systems [29]. FM devices benefit listeners by improving the signal level and signal-to-noise ratio in adverse listening conditions arising from distance from the sound source or in noisy backgrounds. FM systems can be used as primary amplification or linked with other amplification systems. The addition of FM systems early in the amplification fitting process is considered ideal to benefit speech recognition, language development, and academic performance [34]. Guidelines recommend FM systems with BAHA fitting for optimal performance in educational settings [11]. Additional audio adapters in the BAHA Softband allow for direct audio input (DAI) from external audio equipment such as computers, TV, and personal stereo systems to enhance listening for communication and in educational settings [35].
Speech and Language
Studies support that early identification of hearing loss combined with early intervention by age 6 months is associated with typical linguistic development [36]. Moreover, it has been shown that significantly better language outcomes are achieved in children with hearing loss when early identification is joined with early intervention services and active family involvement [37]. In the present case study, baseline assessments at age 1 month revealed delayed speech and language performance. Following coordinated family-centered intervention services including the BAHA Softband fitting along with speech and language therapy within 2 months of age, developmental milestones for auditory comprehension for this child were met by age 7 months. The total language score, which represents both expressive and receptive language skills [24,25] was within normal limits at 19 months. By the last assessment at 25 months the child’s expressive communication showed improvement but did not meet targets for peers without hearing loss. It has been determined that early identification and intervention predicts better language development but does not directly predict speech development outcomes [36].
Family-Centered Intervention
Best practices in the management of pediatric hearing loss includes a collaborative team of professionals and familycentered approach that is culturally and linguistically appropriate [17,29]. The early diagnosis of hearing loss and fitting of amplification are important factors in successful aural habilitation; however, the early initiation of familycentered intervention has been shown to have significant positive impact on language skills in children with hearing loss [38]. Collaboration between health care providers, patients, and their families is a critical element for effective family-centered health care models [39]. Specifically, optimal speech-language therapy practices in children are grounded in a reciprocal co-practice of parents and professionals working together in ‘collaborative practice’ [40].
The presented case study for this child with TCS demonstrated a reciprocal collaborative family-centered intervention model in practice. The parents of the child were actively involved at each hearing and speech service providing input on the child’s performance. For example, amplification functioning was monitored, and adjustments were made using parental feedback including information from questionnaires (ELF). In response to and from consultation with the parents, the audiologist adapted the child’s BAHA Softband fitting to interface with other computer devices.
CONCLUSION
This case study demonstrated successful auditory and language outcomes following early BAHA Softband fitting and coordinated intervention services in a child with TCS and moderately severe CHL due to bilateral aural atresia. The timeframe of assessment and remediation services met the new 1-2-3-month targets recommended by the JCIH [17], where hearing screening is performed by 1 month of age, hearing diagnosis is made by age 2 months, and appropriate intervention begins by 3 months of age. The child presented in this study received medical intervention, hearing diagnosis, and a remediation plan for BAHA Softband fitting along with family-centered EI support services, including speech and language, within 3 weeks following birth. The BAHA Softband was fitted at age 2 months. De- velopmental milestones for language comprehension were met by age 7 months.
These outcomes support that appropriate communicative milestones can be achieved in children with TCS and CHL with early BAHA Softband fitting and a coordinated team management approach involving medical practitioners, au- diologists, speech-language pathologists, early intervention coordinators, family service providers, educators, and parents.
REFERENCES
1. Marszałek-Kruk BA, Wójcicki P, Dowgierd K, Śmigiel, R. Treacher Collins Syndrome: Genetics, Clinical Features and Management. Genes. 2021;12(9):1392.
2. National Institutes of Health. Treacher Collins syndrome. 2020.
3. Trainor PA, Dixon J, Dixon MJ. Treacher Collins syndrome: etiology, pathogenesis and prevention. Eur J Hum Genet 2009;17(3):275-283.
4. Plomp RG, van Lieshout MJ, Joosten KF, Wolvius EB, van der Schroeff MP, et al. Treacher Collins syndrome: a systematic review of evidence-based treatment and recommendations. Plast Reconstr Surg. 2015;137(1):191-204.
5. Thompson JT, Anderson PJ, David DJ. Treacher Collins syndrome: protocol management from birth to maturity. J Craniofac Surg. 2009;20(6):2028-2035.
6. Fuadi FA. Hearing Loss in Treacher-Collins Syndrome. Oto Rhino Laryngologica Indonesiana. 2021; 51(1): 76-81.
7. Marres, HA. Hearing loss in the Treacher-Collins syndrome. Adv Otorhinolaryngol. 2002;61:209-215.
8. Musiek FE, Shinn JB, Baran JA, Jones RO. Disorders of the Auditory System (2nd ed.). Plural Publishing. 2021.
9. Rosa F, Coutinho MB, Ferreira JP, Sousa CA. Ear malformations, hearing loss and hearing rehabilitation in children with Treacher Collins syndrome. Acta Otorrinolaringol Esp. 2016;67(3):142-147.
10. Katsanis SH, Jabs EW, Adam MP, Ardinger HH, Pagon RA, et al. Treacher collins syndrome. In: editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2021. Updated Aug 2020.
11. Snik FM, Mylanus EA, Proops DW, Wolfaardt JF, et al. Consensus statements on the BAHA system: where do we stand at present?. Ann Otol Rhinol Laryngol Suppl. 2005;195:2-12.
12. Hagr A. BAHA: Bone-Anchored Hearing Aid. Int J Health Sci (Qassim). 2007 Jul; 1(2): 265–276.
13. Henry P, Letowski TR. Bone conduction: anatomy, physiology, and communication (No. ARL-TR–4138). Army Research Lab Aberdeen Proving Ground Md Human Research and Engineering Directorate. 2007.
14. Colquitt J, Jones J, Harris P, Loveman E, Bird A. Bone-anchored hearing aids (BAHAs) for people who are bilaterally deaf: A systematic review and economic evaluation. Health Technol Assess. 2011;15(26):1-200.
15. Ellsperman SE, Nairn EM, Stucken EZ. Review of Bone Conduction Hearing Devices. Audiol Res. 2021;11(2):207–219.
16. Roman S. Nicollas R, Triglia JM. Practice guidelines for bone-anchored hearing aids in children. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128(5):253-258.
17. Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. Journal of Early Hearing Detection and Intervention. 2019;4(2):1-44.
18. Verhagen CVM, Hol MKS, Coppens-Schellekens W, Snik AFM, Cremers CWRJ. The BAHA Softband: a new treatment for young children with bilateral congenital aural atresia. Int J Pediatr Otorhinolaryngol. 2005;69(7):973-980.
19. Nicholson N, Christensen L, Dornhoffer J, Martin P, Smith-Olinde L. Verification of speech spectrum audibility for pediatric BAHA Softband users with craniofacial anomalies. Cleft Palate Craniofac J. 2011;48(1):56-65.
20. Polanski JF, Plawiak AC, Ribas A. Hearing rehabilitation in Treacher Collins Syndrome with bone anchored hearing aid. Rev Paul Pediatr. 2015; 33(4): 483–487.
21. Hood LJ. Clinical applications of the auditory brainstem response. Singular Publishing Group, Inc. 1998.
22. Stapells DR, Gravel JS, Martin BA. Thresholds for auditory brain stem responses to tones in notched noise from infants and young children with normal hearing or sensorineural hearing loss. Ear Hear. 1995;16(4):361-371.
23. U.S. Department of Education. (n.d.). Sec. 303.114 Individualized family service plan (IFSP).
24. Zimmerman IL, Steiner VG, Pond RE. Preschool language scales (PLS-4) (4h ed.). Pearson. 2002.
25. Zimmerman IL, Steiner VG, Pond RE. Preschool language scales (PLS-5) (5th ed.). Pearson. 2011.
26. McConnell F, Ward PH. Deafness in Childhood. Vanderbilt University Press. 1967.
27. Anderson KL. ELF: Early listening function. Tampa, FL: Educational Audiology Association. 2002.
28. Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23(7):493-500.
29. American Academy of Audiology. Pediatric Amplification Practice Guidelines. 2013.
30. Hol MK, Cremers CW, Coppens-Schellenkens W, Snik AF. (2005) The BAHA Softband: a new treatment for young children with bilateral congenital aural atresia. Int J Pediatr Otorhinolaryngol. 2005;69(7):973-980.
31. Gelfand S. Essentials of Audiology (3rd ed.). Thieme Medical Publishers, Inc. (2009).
32. Priwin C, Jönsson R, Hultcrantz M, Granström G. BAHA in children and adolescents with unilateral or bilateral conductive hearing loss: a study of outcome. Int J Pediatr Otorhinolaryngol. 2007;71(1):135-1345.
33. Dun CA, de Wolf MJ, Mylanus EA, Snik AF, Hol MK, et al. Bilateral bone-anchored hearing aid application in children: the Nijmegen experience from 1996 to 2008. Otol Neurotol. 2010;31(4):615-623.
34. American Speech-Language-Hearing Association. Guidelines for fitting and monitoring FM systems. 2002.
35. Cire G, Martin RL. Baha, when conventional devices won’t do. The Hearing Journal. 2008; 61(5):46.
36. Yoshinaga-Itano C. From Screening to Early Identification and Intervention: Discovering Predictors to Successful Outcomes for Children With Significant Hearing Loss. J Deaf Stud Deaf Educ. 2003;8(1):11-30.
37. Moeller MP. Early intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):E43.
38. Holzinger D, Fellinger J, Beitel C. Early onset of family centered intervention predicts language outcomes in children with hearing loss. Int J Pediatr Otorhinolaryngol. 2011;75(2):256-260.
39. Kokorelias KM, Gignac M, Naglie G, Cameron JI. Towards a universal model of family centered care: a scoping review. BMC Health Services Research. 2019; 19(1):564.
40. Klatte IS, Lyons R, Davies K., Harding S, Marshall J, et al. Collaboration between parents and SLTs produces optimal outcomes for children attending speech and language therapy: Gathering the evidence. Int J Lang Commun Disord. 2020;55(4):618-628.
Article Information
Article Type: Case Report
*Corresponding author
Diane Davis, Department of Communication Sciences and Disorders, Adelphi University, 158 Cambridge Avenue, Hy Weinberg Center 133, Garden City, NY 11530-0701, Office: 516-877-4773
Received: April 04, 2023; Accepted: April 12, 2023; Published: April 15, 2023
CC: This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.
Cite as: Davis D, Serpanos YC. Early Intervention Case Study: Bone-Anchored Hearing Aid (BAHA) Softband Fitting in Treacher Collins Syndrome. J Commun Disorder Assist Technol. 2023; 4: 1-9.



