Idiopathic Normal pressure Hydrocephalus. How Much Are We Missing
Shoukry EE, M.D
SUMMARY
Normal pressure hydrocephalus (NPH) IS a type of brain malfunction caused by expansion of the lateral ventricles with distortion of the corona radiate fibers. The pathophysiology of idiopathic Normal pressure hydrocephalus remains unclear but is considered to be a communicating hydrocephalus due to reduced CSF absorption. It is theorized that shearing stress forces are exerted on periventricular vessels leading to ischemic changes or it is possibly secondary to interstitial edema with impaired blood flow. It was first described by Hakim and Adams in 1965 [1]. There are 2 types of NPH: Idiopathic (iNPH) and secondary to trauma, tumor, subarachnoid hemorrhage, meningitis…etc. [2]. Symptoms are summarized by Hakim’s triad of gait disorder, dementia and urinary incontinence or “Weird Walking Water”.
Gait is usually slow, wide based, with foot dragging (magnetic gait) and outwardly rotated feet. Motion in joints is reduced and arm swing can be exaggerated. Falls are common, usually backwards, and is sometimes compensated by a forward leaning posture of the trunk [3]. Idiopathic NPH can be described as lower body Parkinsonism, with no rigidity or tremors.
Dementia is frontal lobe, subcortical in type with inattention, apathy, forgetfulness, dullness in thinking and actions [4].
Urinary incontinence occurs late in the course of the disease, is usually urgency in type and secondary to removal of supraspinal inhibition with detrusor over activity [4].
Prevalence of NPH among residents of assisted living facilities was estimated to range between 9-14% [5].
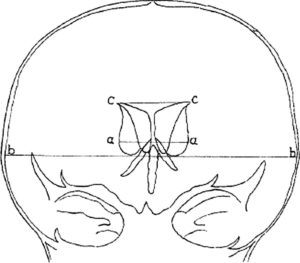
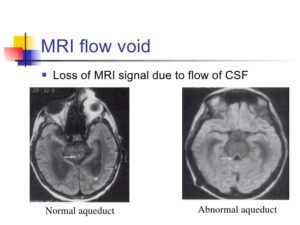
CT scan head is usually used as a screening tool and is one of the reason CT scan is ordered with cognitive impairment or recurrent falls, however its sensitivity and specifity to detect iNPH is unknown. Ventriculomegaly out of proportion to sulcal enlargement has been historically quantified by Evans index (transverse diameter of frontal horns of the lateral ventricle divided by transverse diameter of the skull , usually above 0.3) but is far from being an ideal measurement as it depends on the level at which frontal horns and inner skull diameters are measured (Figure 1). MRI brain is the best modality to diagnose iNPH. Beside ventriculomegaly, it may show periventricular high signal on T2 weighted sequences reflective of trans ependymal migration of CSF [6], thinning of corpus callosum and aqueductal flow void due to increased CSF velocity across the aqueduct of Sylvius, where the CSF appears black on T2 weighted images (Figure 2). Nuclear medicine Cisternography and CT Cisternography are less important in diagnosing iNPH.
Figure 1: Evans’ index revisited
Note: Evans Index= cc/bb and is normally less than 0.3 [7].
Figure 2: Normal-pressure-hydrocephalus
High volume lumbar puncture (Miller Fisher test) where at least 30 ml of CSF is removed should be done in all patients with suspicion of iNPH. It usually showed an opening pressure in the high range of normal limits, i.e. 150-200 mmH2O. Gait before and after lumbar puncture should be tested as it has prognostic implications and can predict success of shunting procedure. However, it has low negative predictive value, i.e. lack of improvement in gait speed doesn’t rule out the diagnosis of iNPH.
External Lumbar drainage (ELD), when an intrathecal catheter is inserted allowing drainage of CSF for 3- 4 days , has the highest sensitivity and specifity to diagnose the condition but carries a risk of infection and catheter dislodgement. Infusion test when Ringer lactate solution is infused via an intrathecal catheter while continuously monitoring pressure is another option permitting the measurement of outflow conductance (Cout). Continuous Intracranial pressure monitoring may identify patients who would benefit the most from shunt placement and shows intermittent intracranial hypertension in some patients.
Prognostic tests such as Miller Fisher test, ELD and infusion test sometimes yield false results if CSF is altered by severe spinal stenosis [8]. This is particularly important since both cervical and lumbar spinal stenosis can both be in the differential diagnosis of iNPH and may need to be ruled out.
Once the diagnosis of iNPH is established, a shunting procedure, usually a ventriculoperitoneal (VP) shunt is considered. Ventriculomegaly will diminish 3-4 days after placement of the shunt, however only 21% will show marked improvement in symptoms, usually those with gait disturbances, mild or no urinary incontinence and mild dementia. More recent studies showed that if patients with iNPH, shunt placement yielded beneficial outcomes in 86% of patients (81% in gait disturbances, 70% in urinary incontinence and 40% in cognitive impairment) [9,10].
Both CSF biomarkers [11] and Neuroimaging in general could not predict the ELD outcome, although there is possibly a role for soluble Amyloid precursor protein (APP) alpha in CSF [12]. CSF biomarkers are mainly used to rule out associated disease, e.g. Alzheimer’s disease.
In summary, the prevalence of the disease, lack of biomarkers and/or specific neuroimaging findings, and favorable outcome to shunting procedure in a well selected population should guide our assessment in patient with gait disturbances, as follows:
- Our target should be the population above 65 Y old where the incidence of iNPH is about 0.5%, with peak onset in 6th and 7th decades [13]. A large Norwegian study showed a significant increase in incidence with increasing age (3.3 per 100K for people 50-59 Y of age, up to 181.7 per 100K for people 70-79 Y of age [14].
- Selection of ideal patients for shunting procedure is crucial. Favorable prognostic factors include [14]:
-short duration of symptoms (less than 6 months)
-onset of gait abnormality preceding dementia
-temporary symptom relief after high volume Lumbar puncture, especially gait
-absence of significant cerebrovascular disease
-aqueductal flow void on T2 weighted images.
Given the facts outlined above, one has to wonder how many patients with iNPH, potentially reversible disease, are missed, especially in the elderly population with gait disturbances/recurrent falls who end up in assisted living or Skilled nursing facilities.
REFERENCES
- Adams, R, Hakim S. Symptomatic occult hydrocephalus with normal CSF pressure. N Engl J Med. 1965; 273: 117-126.
- National Institute of Neurological disorders and Stroke. NINDS. 2011.
- Blomsterwall E, Svantesson U, Carlsson. Postural disturbances in patients with normal pressure hydrocephalus. Acta Neurol Scand. 2000; 102: 284-291.
- Younger DS. Adult normal pressure hydrocephalus in motor disorders (2nd edition), pages, Philadelphia PA, Lippincott Williams and Wilkins. 2005; 581-584.
- Marmarou A, Young HF, Aygok GA. Estimated incidence of normal pressure hydrocephalus and shunt outcome in patients residing in assisted living and extended care facilities. Neurosurg focus. 2007; 22: 1-8.
- Tarnaris A, Toma AK, Kitchen ND, Watkins LD. Ongoing search for diagnostic biomarkers in idiopathic NPH. Biomark Med. 2009; 787-805.
- Toma AK, Holl E, Kitchen ND, Watkins LD. Evans’ index revisited: the need for an alternative in normal pressure hydrocephalus. Neurosurgery. 2011; 68: 939-944.
- Komotar RJ, Zacharia BE, Mocco J, Kaiser MG, Frucht SJ. Cervical spine disease may result in negative lumbar spinal drainage trial in NPH: Case report. Neurosurgery. 2008; 63: 315.
- Vanneste J, Augustin P, Dirven C, Tan WF, Goedhart ZD. Shunting normal-pressure hydxrocephalus: Do the benefits outweigh the risks? A multicenter study and literature review. Neurology. 1992; 42; 54-59.
- Poca MA, Mataro M, Del Mar Matarín M, Arikan F, Junqué C, et al. Is the placement of shunts in patient with idiopathic NPH worth the risk? Results of a study based on continuous monitoring of ICP. J Neurosurgery. 2004; 100: 855-866.
- Leinonen V, Menon LG, Carroll RS, Iacono DD, Grevet J. CSF biomarkers in idiopathic NPH. Int J Alzheimers Dis. 2011; 6.
- Pyykko OT, Lumela M, Rummukainen J, Nerg O, Seppala T, et al. PLoS One. 2014; 9: 3, 0-91974.
- Brean A, Eide PK. Prevalence of of probable idiopathic NPH in Norwegian population, Acta Neurol Scand. 2008; 118; 48- 53.
- Hurley RA, Bradley WG, Latifi HT. Normal pressure hydrocephalus, Significance of MRI in a potentially treatable Dementia. J Neuropsychiatry Clin Neurosci. 1999,11; 297-300.
* Corresponding author: Emad Essam Shoukry, Division of Geriatrics, University of North Texas Health Science Center, United States, E-mail: Emad.Shoukry@unthsc.edu
Received: Mar 08, 2017; Accepted: Mar 14, 2017; Published: Mar 16, 2017
CC: This article is distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use and redistribution provided that the original author and source are credited.
Competing interests: The authors have declared that no competing interests exist.
Cite as: Shoukry EE. Idiopathic Normal pressure Hydrocephalus. How Much Are We Missing. J Ageing Disabil Chronic Dis. 2017; 1: 1-5.